It has often been estimated that it takes, on average, 17 years to translate a novel research finding into routine clinical practice. This time lag is due to a combination of factors, including the need to validate research findings, the fact that clinical trials are complex and take time to conduct and then analyze, and because disseminating information and educating healthcare workers about a new advance is not an overnight process.
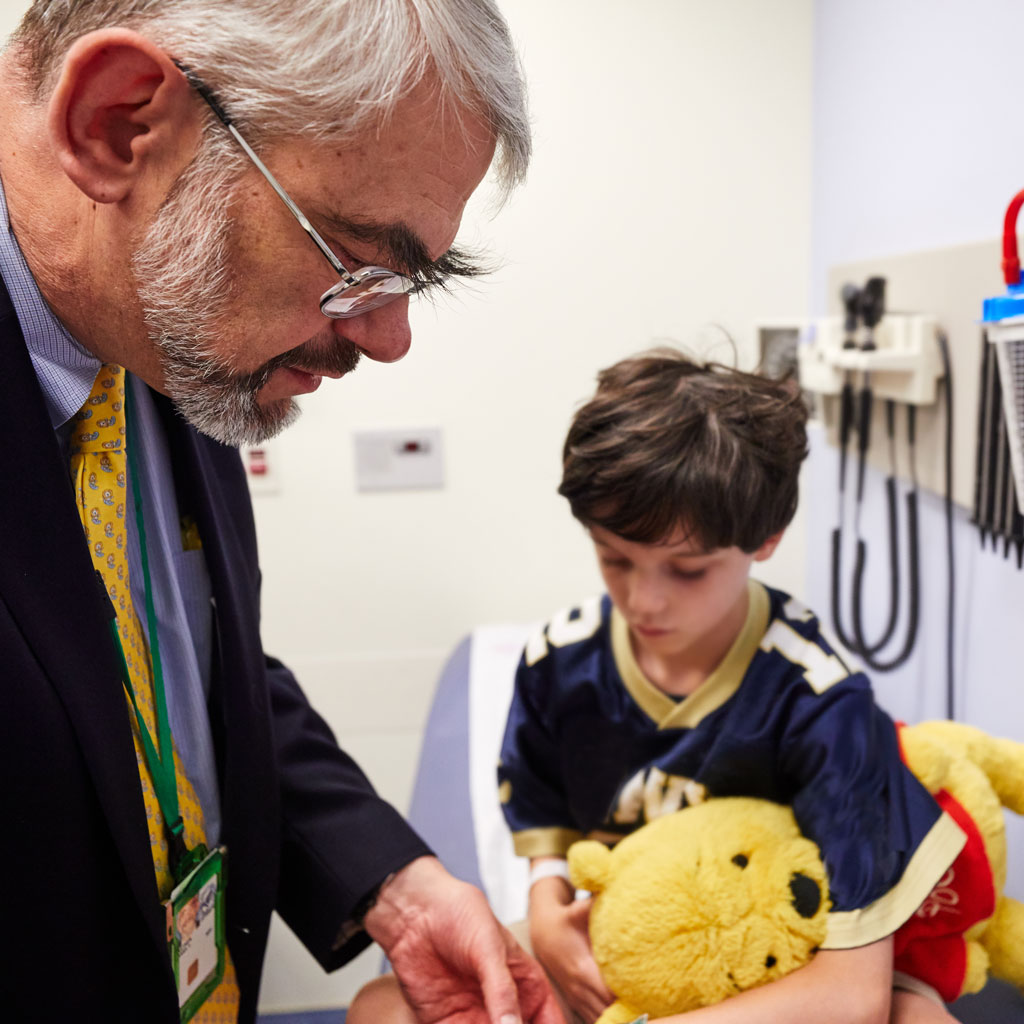
Once sufficient evidence has been generated to demonstrate a benefit to patients, or "clinical utility," professional societies and clinical standards groups will use that evidence to determine whether to incorporate the new test into clinical practice guidelines. This determination will also factor in any potential ethical and legal issues, as well economic factors such as cost-benefit ratios.
The NHGRI Genomic Medicine Working Group (GMWG) has been gathering expert stakeholders in a series of genomic medicine meetings to discuss issues surrounding the adoption of genomic medicine. Particularly, the GMWG draws expertise from researchers at the cutting edge of this new medical toolset, with the aim of better informing future translational research at NHGRI. Additionally the working group provides guidance to the National Advisory Council on Human Genome Research (NACHGR) and NHGRI in other areas of genomic medicine implementation, such as outlining infrastructural needs for adoption of genomic medicine, identifying related efforts for future collaborations, and reviewing progress overall in genomic medicine implementation.