Last updated: March 22, 2012
Sequencing Insights Into Multiple Myeloma
Genome Advance of the Month
Sequencing Insights Into Multiple Myeloma
March 2011
By Jonathan Gitlin, Ph.D.
Science Policy Analyst
Cancer is a genetic disease. Period.
Some inherited forms of cancer run in families, but genomic mistakes accumulated during life — such as those from exposure to chemicals in cigarette smoke, or from a stray bit of cosmic radiation, or random mistakes in DNA duplication — are the cause of most tumors.
That's why the National Human Genome Research Institute (NHGRI) partnered with the National Cancer Institute (NCI) in 2005 to launch The Cancer Genome Atlas (TCGA), a large-scale effort to map the disease-causing genetic changes in the most widely recognized cancers, of which there are more than 200 types.
Even as the work of TCGA progresses, other research teams from around the world use genome-wide analyses to hunt down the genetic roots of cancer. For the March Genome Advance of the Month, NHGRI has selected a study that shows how the power of sequencing technology has generated an important discovery, even when studying a relatively small number of patients, in this case only 38. TCGA studies, on the other hand, include 500 patients in the analyses of each tumor type.
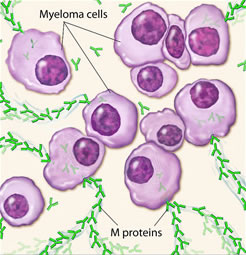
The study, published in the March 24, 2011 issue of the journal Nature, describes how a nationwide team of researchers organized by Todd R. Golub, M.D., director of the cancer program at The Eli and Edythe L. Broad Institute in Cambridge, Mass., made several new discoveries about the genetic causes of multiple myeloma, a currently incurable form of cancer that affects a type of immune cell called a B lymphocyte. More than 20,000 Americans develop multiple myeloma each year; about half that number die from the disease annually.
The researchers used whole-genome sequencing in 23 patients and whole-exome sequencing, where just the protein-coding regions of the human genome are sequenced, in 16 patients. One patient was studied with both techniques. The researchers compared the sequence of the DNA in each patient's tumor to their normal DNA. By comparing tumor DNA to normal DNA, the researchers discovered around 2.9 mutations for every million bases of DNA. This resulted in nearly 7,500 point mutations across the genome, 35 of which change amino acids in proteins, as well as 21 chromosomal rearrangements that affect regions that code for proteins. The mutations were many times more likely to happen to C or G bases (rather than As or Ts), and less common in regions that code for proteins (exons) compared to introns or regions between genes. The researchers found that ten genes in particular showed significant rates of mutations, including six that had never previously been linked to cancer.
One particular mutation, in an enzyme called BRAF, may quickly lead to clinical treatment with existing medications that inhibit BRAF; however, only a small subset of multiple myeloma patients had this mutation. Also, in nearly half of the patients, the researchers discovered mutations in genes involved in processing RNA, the translation of RNA into protein, and the subsequent folding of proteins, suggesting many possible targets for future therapies.
The results suggest, the researchers wrote, that sequencing studies will produce "new insights into cancer not anticipated by existing knowledge." Genomics has the potential to have a positive impact on many areas of medicine, but the most immediate are likely to be achieved in more accurately diagnosing an illness, in pharmacogenomics (tailoring drug treatment to a patient's DNA) and in cancer care.
Read the study: Initial genome sequencing and analysis of multiple myeloma. Nature, March 24, 2011
In March there were also other interesting developments in the field, grouped and summarized below.
Clinical Advances:
- Human Genome Sciences, a Maryland-based pharmaceutical company, and its development partner GlaxoSmithKline, won FDA approval for the first new drug to treat lupus in over 50 years.
- A team at Stanford Medical School identified several new risk loci in cardiovascular disease: Large-scale association analysis identifies 13 new susceptibility loci for coronary artery disease. Nature Genetics, March 6, 2011
- Macular degeneration can be caused by a buildup of RNA elements, according to a group at the University of Kentucky: DICER1 deficit induces Alu RNA toxicity in age-related macular degeneration. Nature, March 17, 2011
Evolutionary biology:
- A new evolutionary history of primates: A Molecular Phylogeny of Living Primates, PLoS Genetics, March 17, 2011
- Humans vs chimpanzees: identifying the genetic changes that separate the species: Human-specific loss of regulatory DNA and the evolution of human-specific traits. Nature, March 9 2011