More widespread access to genomic medicine vital for studying a rare, underdiagnosed blood disorder
Scientists are exploring the genomic and clinical profiles of people with RUNX1 familial platelet disorder.
A few years ago, Emily* discovered that she had fewer platelets in her blood than most people. Platelets, sticky disc-shaped pieces of cells, form clots to stop bleeding and help wounds heal.
She had always bruised easily, but it just seemed like a curiosity that ran in her family.
However, when one of Emily’s relatives underwent genetic testing for an unrelated condition, they were told that they also had a variant of a gene called RUNX1 that was associated with a platelet disorder.
The pieces started to come together for Emily. She reached out to other relatives, learning that there were more diagnoses in her extended family that had not been communicated to others.
“We realized that we had another cousin with a RUNX1 variant diagnosis in the last year, but they didn’t reach out to us,” she said. “When we talked to our uncle, he said we had more relatives with the disorder.”
While Emily was curious about her own status, she felt nervous that she would discover she also had a variant form of RUNX1. associated with the condition. Other than easy bruising and bleeding as well as low platelets, she felt okay. Ultimately, she decided knowing is better than not knowing and to not let fear get in the way.
Many of Emily’s doctors have never heard of RUNX1 familial platelet disorder (RUNX1-FPD), let alone know how to recognize the signs and symptoms. In Canada where Emily lives, genetic testing to diagnose such a condition is not part of standard care.
She had hit a roadblock until she happened to speak with her aunt, who works at the National Institutes of Health (NIH).
Thanks to her aunt, Emily found the NIH RUNX1-FPD clinical research study, which takes a detailed look at the clinical and genetic features of people who may have the rare condition. She enrolled in the program and sent her DNA for testing.
When the results came back two weeks later, they confirmed that she had the familial RUNX1 variant and was diagnosed with RUNX1-FPD.
*last name omitted for privacy
A disorder of the blood
Although researchers have known for more than 20 years that genomic variants in the RUNX1 gene cause the disorder, it is still poorly understood partly because of its variable symptoms and the lack of detailed research about the disorder.
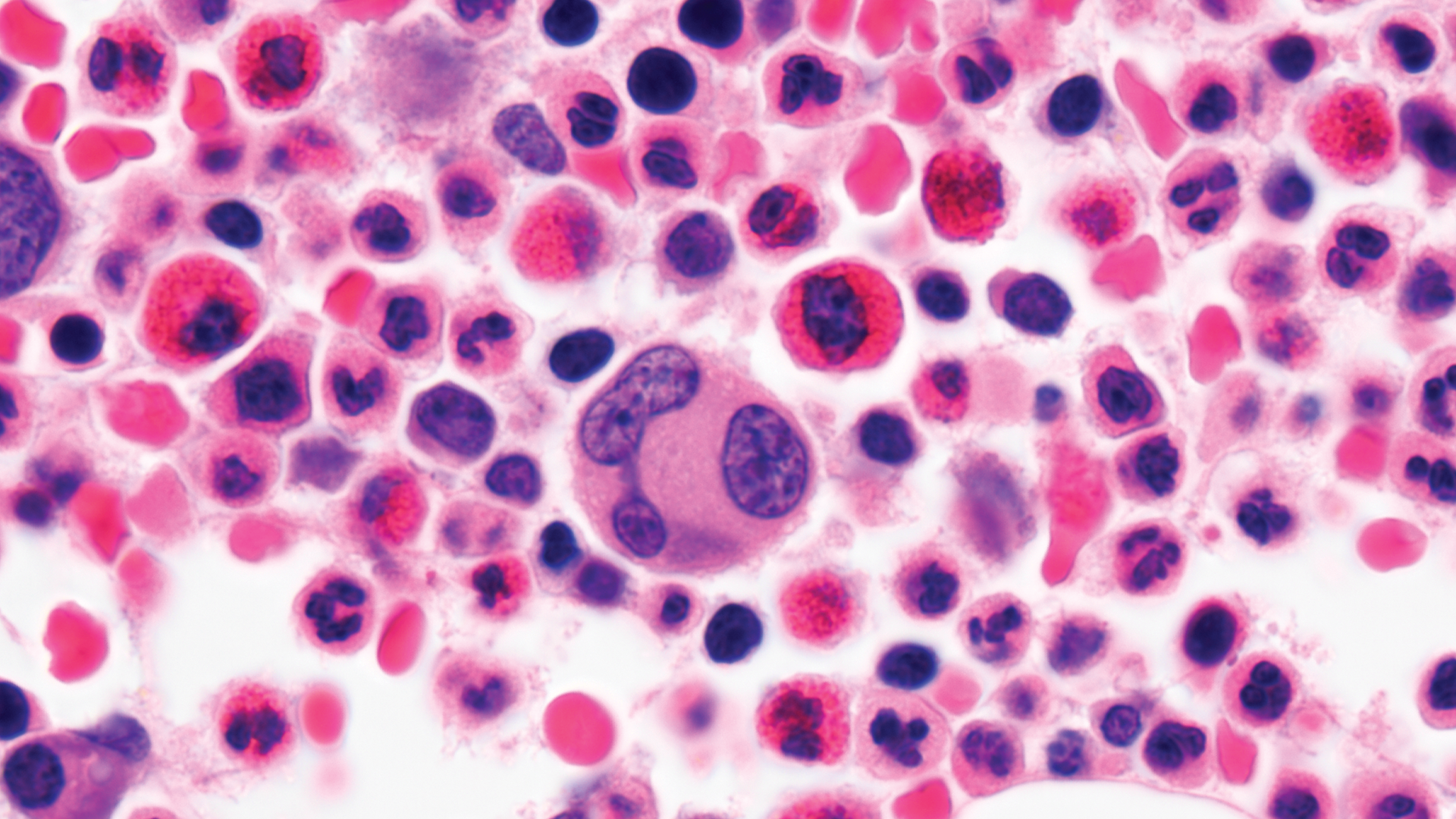
The RUNX1 gene codes for a transcription factor, which turns genes on and off. It also helps stem cells in the blood, known as hematopoietic stem cells, develop and function. These stem cells generate all types of blood cells, such as red blood cells, white blood cells and platelets.
Variants in the RUNX1 gene lead to faulty or incomplete proteins that do not function optimally. With an altered RUNX1 protein, platelets do not develop as expected, resulting in fewer or less-functional platelets.
People with RUNX1-FPD typically have lower platelet counts, prolonged bleeding and easy bruising, which can cause problems during surgeries. The disorder is also associated with a higher chance of developing blood cancers, such as myelodysplastic syndrome, acute myeloid leukemia and acute lymphoblastic leukemia. Many people with this disorder may also have skin conditions, such as eczema.
Paul Liu, M.D., Ph.D., senior investigator within the Translational and Functional Genomics Branch at the National Human Genome Research Institute (NHGRI), who has led an NIH research group investigating this condition for more than a decade, recently publishing two papers about their clinical and genomic studies of RUNX1-FPD.
"Our study represents the largest prospective cohort of participants with RUNX1 variants, which allows us to deepen our knowledge of the disorder and discover new clinical findings associated with people with the disorder,” says Dr. Liu.
How the disorder progresses and what happens at a genomic and cellular level has not been deeply examined until now, according to Dr. Liu.
Natalie Deuitch, M.S., a genetic counselor at NHGRI and part of the group conducting the NIH RUNX1 clinical study, says they closely monitor families with RUNX1 variants to understand how the disorder progresses with the hopes of developing new therapies.
“We wanted to understand the full extent of what happens with RUNX1-FPD,” said Deuitch. “What other symptoms have other researchers not looked at before? Are there features that might predict if someone would develop leukemia?”
A collection of clinical features
In the first study, published in the journal Blood, the researchers followed over 100 participants with RUNX1 variants, analyzing their genome, blood, bone marrow and other systems. The participants were enrolled if they had proven or suspected RUNX1 variants due to their symptoms or family history of bleeding issues and/or cancer. RUNX1-FPD is an autosomal dominant condition, so within each family, there are typically multiple affected individuals. Many family members of participants were also part of the study since they, too, had the disorder.
The researchers found that most of the participants had fewer platelets and abnormal platelet function. Half of them had abnormal bleeding. Many participants had allergy symptoms (e.g., eczema, allergic conjunctivitis and asthma) and gastrointestinal symptoms (e.g., acid reflux, constipation and difficulties swallowing). These clinical manifestations haven’t been well evaluated in people with RUNX1-FPD, according to Deuitch. The researchers also found a few clinical features in the bone marrow that may help clinicians diagnose the disorder.
“I was surprised by how variable this condition is,” said Deuitch. “Two people with the exact same genetic change can have vastly different experiences with this disorder.”
Around 60% of the participants have at least one family member who developed a hematologic malignancy. Sixteen percent of the participants had been diagnosed with cancer or a precancerous condition, most of which do not respond or stop responding to treatment after some time, with many of the participants requiring hematopoietic stem cell transplantation.
“The results of this study can help pathologists and hematologists become aware of what RUNX1-FPD might look like and can help them identify potential new cases,” she said.
Looking for clues in the genome
The second study from Dr. Liu’s group, published in Blood Advances, looked deeper into the genomics underlying the condition.
The researchers examined different RUNX1 variants found in over 60 participants and how they relate to symptoms and laboratory results, including how changes in other parts of the genome can affect a person’s risk of developing leukemia.
By conducting exome sequencing, which analyzes the coding portion of the genome, as well as RNA sequencing and genotyping, which analyze gene activity and genomic structural changes, respectively, the researchers found 28 different genomic RUNX1 variants in the 29 families. These variants ranged from smaller changes in the RUNX1 gene to larger changes that affected a bigger portion of the gene.
The researchers also analyzed the exome sequences of participants to look for both somatic and germline RUNX1 variants. Somatic genomic changes are those that happen in just some cells in the blood and bone marrow over time. These changes may indicate that a person is starting to develop leukemia. People with RUNX1-FPD seem to accumulate these variants more frequently and at earlier ages than the general population.
The researchers also looked for germline RUNX1 variants (those that are typically inherited and present in nearly every cell in the body) to try to understand if there may be other genomic factors that could increase or decrease the risk of developing leukemia. More data will be needed to make any strong conclusions about the effects of these genomic factors, but this paper is an important first step.
“Studying the genomic landscape of this population helps patients understand their lifetime risk of developing leukemia,” said Deuitch. “By getting a more accurate estimate of a person’s risk of developing leukemia, we can hopefully perform fewer laboratory tests for those at lower risks and more tests for those at higher risks in order to identify the leukemia earlier.”
A call for more awareness and access to genetic testing
Currently, more than 250 families have been identified to have RUNX1 variants. Although considered a rare disorder, many researchers and clinicians believe that RUNX1-FPD is severely underdiagnosed.
“Many of the participants in our study had their diagnosis picked up by secondary findings or because patients really advocated for their doctors to order genetic testing,” said Deuitch. “When I look at the previous medical records of these patients, it seems obvious to me that they have RUNX1-FPD — all the pieces fit together. But they’re falling through diagnostic cracks.”
Clinicians, oblivious to the genetic condition, may not be able to properly diagnose RUNX1-FPD patients due to lack of training in genomic medicine. Furthermore, not everyone can access genetic testing due to cost or lack of health insurance. Lastly, genetic reference databases that a patient's genetic results are compared to are currently not very diverse because they mostly consist of reference genomes from people of European ancestry. This current lack of ancestral diversity may hinder scientists’ and clinicians’ ability to provide equitable care across different population groups.
Without finding the study to join, Emily would not have discovered her diagnosis.
“It’s an amazing program. I’m getting all sorts of healthcare that wouldn’t otherwise be available to me. I’m learning a lot about myself through the tests that they’re doing for us,” she said.
Emily hopes that more clinicians will become educated about genomic medicine, so that people with RUNX1-FPD will know about their health risks, though she understands the fear of living with such a diagnosis.
“It’s important to learn as much as possible about the disorder but not get swallowed up by it,” said Emily. “I’m taking it day-by-day and not letting my diagnosis get in the way of enjoying life. None of us knows what the future holds, and having the diagnosis is just another factor.”
The RUNX1 clinical trial program is still recruiting participants. Visit the webpage for more information on eligibility.
Last updated: February 28, 2024
