For skeletal genomicist Carlos Ferreira, answers are in the bones
With hundreds of rare bone disorders catalogued and more to be discovered, Dr. Ferreira discusses the challenges of skeletal genomics.
Soo: What was your path to becoming a clinician and a researcher?
Ferreira: Initially, I wanted to be a physicist or a mathematician. During my last year of high school, I decided to pursue a career in medicine because I found it challenging and stimulating and because I wanted to make a difference in people’s lives. In my home country of Paraguay, you go from high school directly to medical school. I have to say that I have never regretted making that decision so early, specifically, at the age of 18.
The idea to become a researcher came much later, when I was already in the U.S. finishing my training in medical genetics. After being exposed to clinical research here at NHGRI and other institutions nearby, I knew it was a good fit for me, and I was hoping to help patients with rare disorders.
Soo: What was it like growing up in Paraguay?
Ferreira: I was born and raised in Asunción as part of a loving and supportive family. There was a huge degree of income inequality there, and my parents struggled to send all four of their children to school. For the first decade of my life, the country was ruled by a dictatorship, and when a coup d’état ensued in 1989, there was still a degree of constant fear and uncertainty.
There wasn't a lot of room for genetics in Paraguay. Back then, there was only one geneticist for about seven million people, so it was very underserved. We would often make working diagnoses because we wouldn’t be able to order tests or confirm diagnoses because of the lack of resources. That’s actually what prompted me to come to the U.S. after completing medical school.
Soo: What was your experience getting into the genetics field?
Ferreira: I knew I wanted to be a geneticist, but I thought it would be very hard for me to match in a genetics training program. So, I applied to internal medicine first. I thought my chances of getting a position and residency as an international medical graduate would have been better. I did an internal medicine residency in Chicago. Once you're on U.S. soil, everything is easier because people get to know you.
I did apply eventually for medical genetics training, and I matched here at NHGRI. The rest is history. I fell in love with clinical research, and I decided to pursue a career specifically in something called the Physician-Scientist Development Program, which allows you to basically start as a junior faculty in a pre-tenure track program with a mentoring committee and stable funding, then later apply for tenure track positions. It's kind of a convoluted path, but that's how I got here.
Soo: Were there any challenges on your path to becoming a researcher?
Ferreira: In my case, I trained as a physician, but not in the U.S. It was a steep learning curve for me, not having a Ph.D. and having to learn not only the basic technologies, but also some novel technologies that appear all the time.
I eventually learned how to extract DNA and even develop my own bioinformatics analyses. But these are not things that happen overnight. The NHGRI environment provided me stable funding and time to focus and learn.
Soo: What are you studying in your skeletal genomics unit?
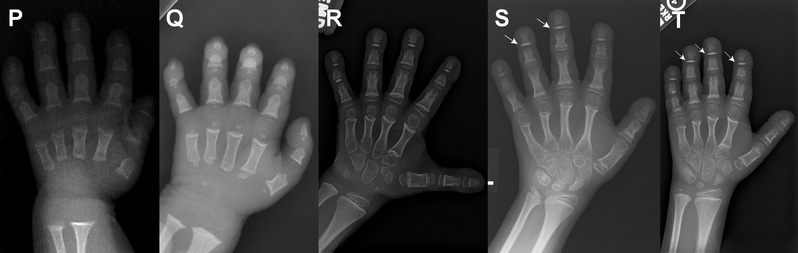
Ferreira: We study specific rare skeletal disorders, and we have a few different goals. We’re trying to discover new associations between genes and disorders. We are also establishing cell and animal models to study these new genes that are associated with abnormal skeletal physiology and skeletal disorders. Finally, we’re trying to find new therapeutic approaches for some of these genetic disorders, with the hope that these preclinical studies will eventually lead to clinical trials and decrease the burden of disease of our patients.
Soo: What are some difficulties in understanding skeletal disorders?
Ferreira: Some challenges are inherent to the research itself. It’s very hard to obtain skeletal samples, such as from bone or cartilage, other than by invasive surgery. You can get some information from, for example, blood samples. But in some cases, the disorders are mosaic, meaning that only certain tissues are affected.
Also, for disorders that are rare, it’s not easy to find patients. Sometimes, we might be dealing with conditions that have only been seen in one or two dozen patients in the history of medicine.
Soo: Your group was the first to uncover the cause of Saul-Wilson syndrome and characterize the disorder. What are some key findings?
Ferreira: We found that all patients with Saul-Wilson syndrome have the same genomic changes and similar clinical signs and symptoms. The disorder is very rare — only four patients were described in the ’80s and ’90s, and then no new diagnosis were made for around the next quarter century. When the first patient came to our clinic, we found their disease-causing genomic variant and looked for other patients with the same variant. Within a week or so, we were able to diagnose seven patients. I think that was one of the big successes I’ve had in the field of skeletal dysplasia.
Soo: What other discoveries have your group made?
Ferreira: We also characterized patients with generalized arterial calcification of infancy, starting with a natural history study in collaboration with other groups. We had the largest cohort ever described, and we have been able to learn about the prognosis and different symptoms associated with this disorder.
Another key project involves studying osteoglophonic dysplasia, a rare disorder that is caused by a genomic variant in a specific receptor and characterized by abnormal bone growth in the head and face. We have a mouse model that recapitulates the human disease, and we are in the process of running a clinical trial to test a drug that acts on the receptor.
Soo: What are you looking forward to on the horizon of genetics and genomics?
Ferreira: I’m hoping to incorporate new genomic technologies and try new therapies for patients. There are hundreds of rare skeletal disorders, but we don’t have treatment for even 5% of these disorders. Even the more common disorders are just starting to have proposed treatments. There are many therapies and approaches currently being developed, such as gene therapy and the use of small molecules. By improving our understanding of these disorders and trying new therapies, I hope we can make a difference in the lives of these patients.
Last updated: August 14, 2023