To understand sickle cell disease and gene therapy, you should first know about blood cells and the different types of hemoglobin that make up red blood cells.
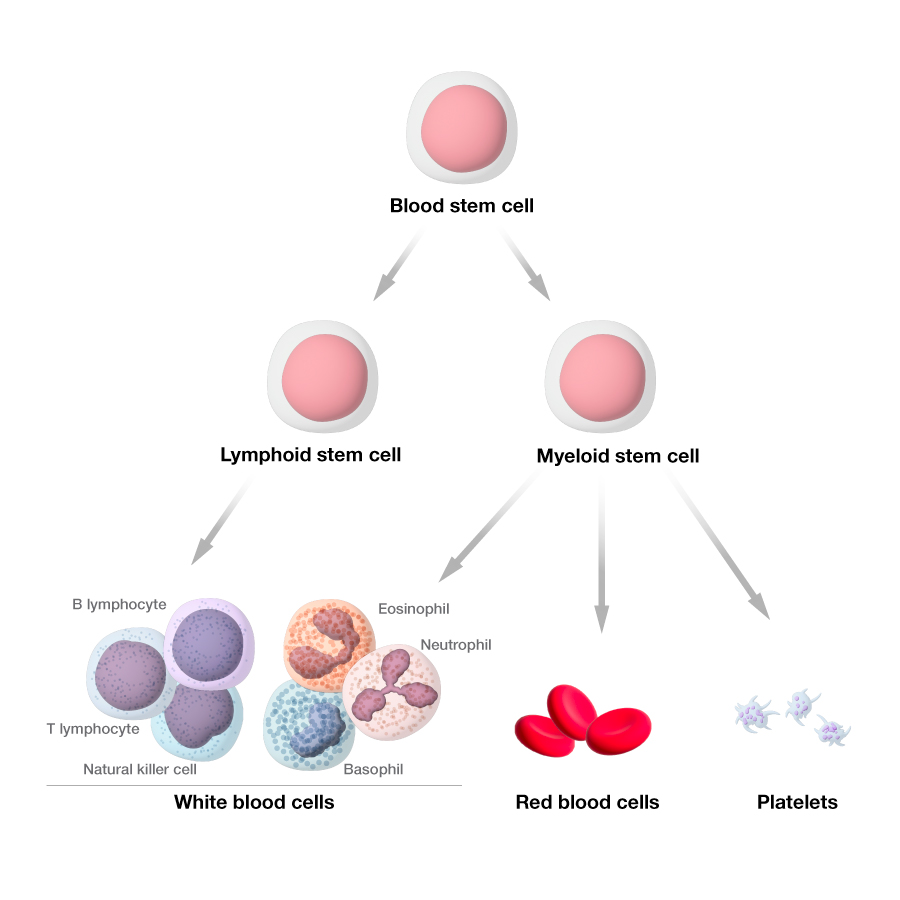
Blood stem cells and blood cell development
Blood stem cells (also called hematopoietic stem cells) are cells that can develop into any type of blood cell in your body, such as white blood cells, red blood cells and platelets. Blood stem cells live and divide in your bone marrow.
White blood cells are part of the body's immune system; they help the body fight infection and other diseases. Platelets are important in blood clotting. Your physician will monitor your white blood count and platelets.
Different therapies are designed to treat or relieve the symptoms of sickle cell disease by targeting your blood stem cells.
Hemoglobin types and sickle cell disease
Your red blood cells contain hemoglobin, a protein that carries oxygen. Red blood cells need hemoglobin to deliver oxygen to your body’s organs and tissues. Every red blood cell contains thousands of hemoglobin molecules.
The genes in our body code for different types of hemoglobin. We will focus on three types:
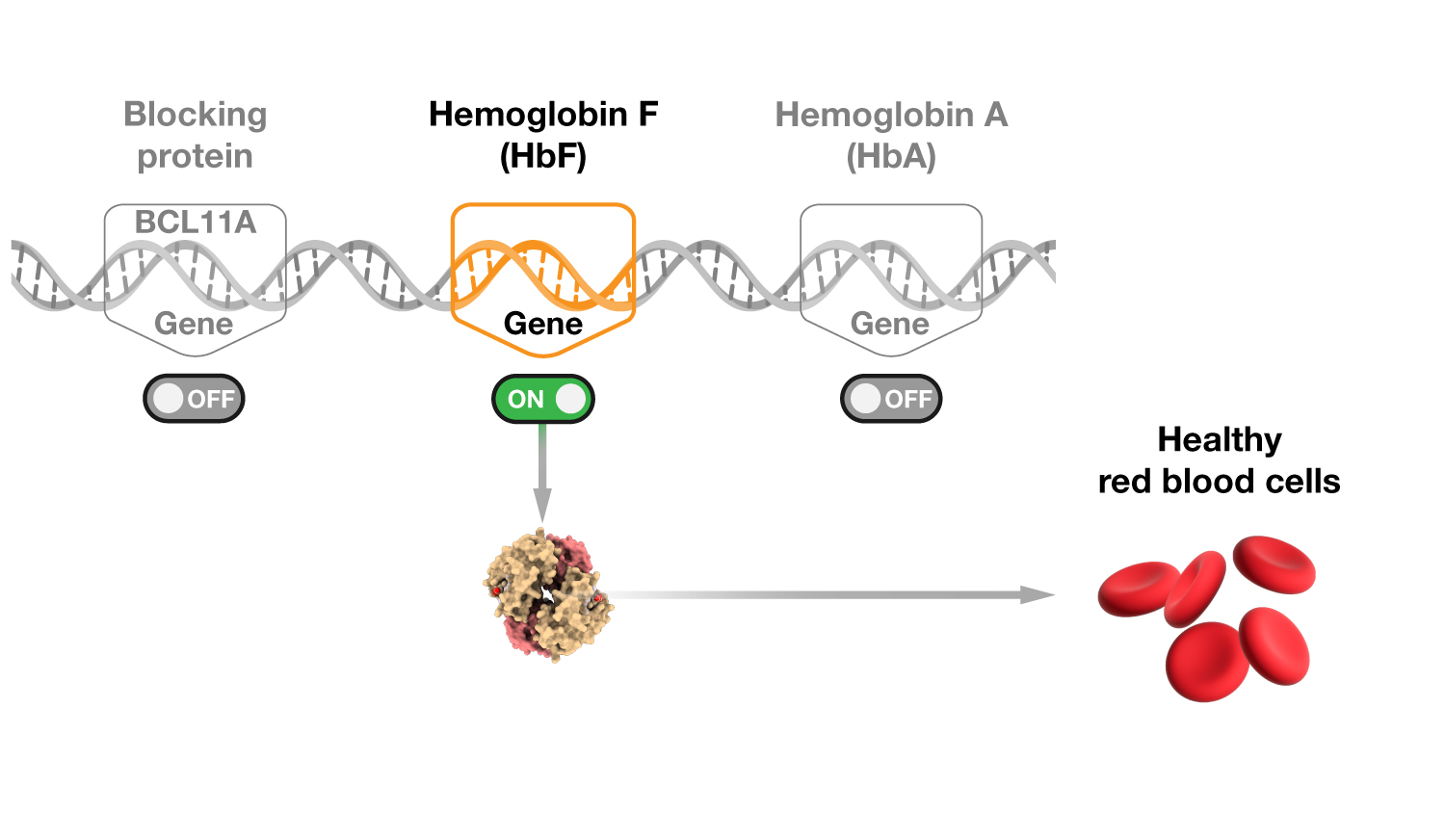
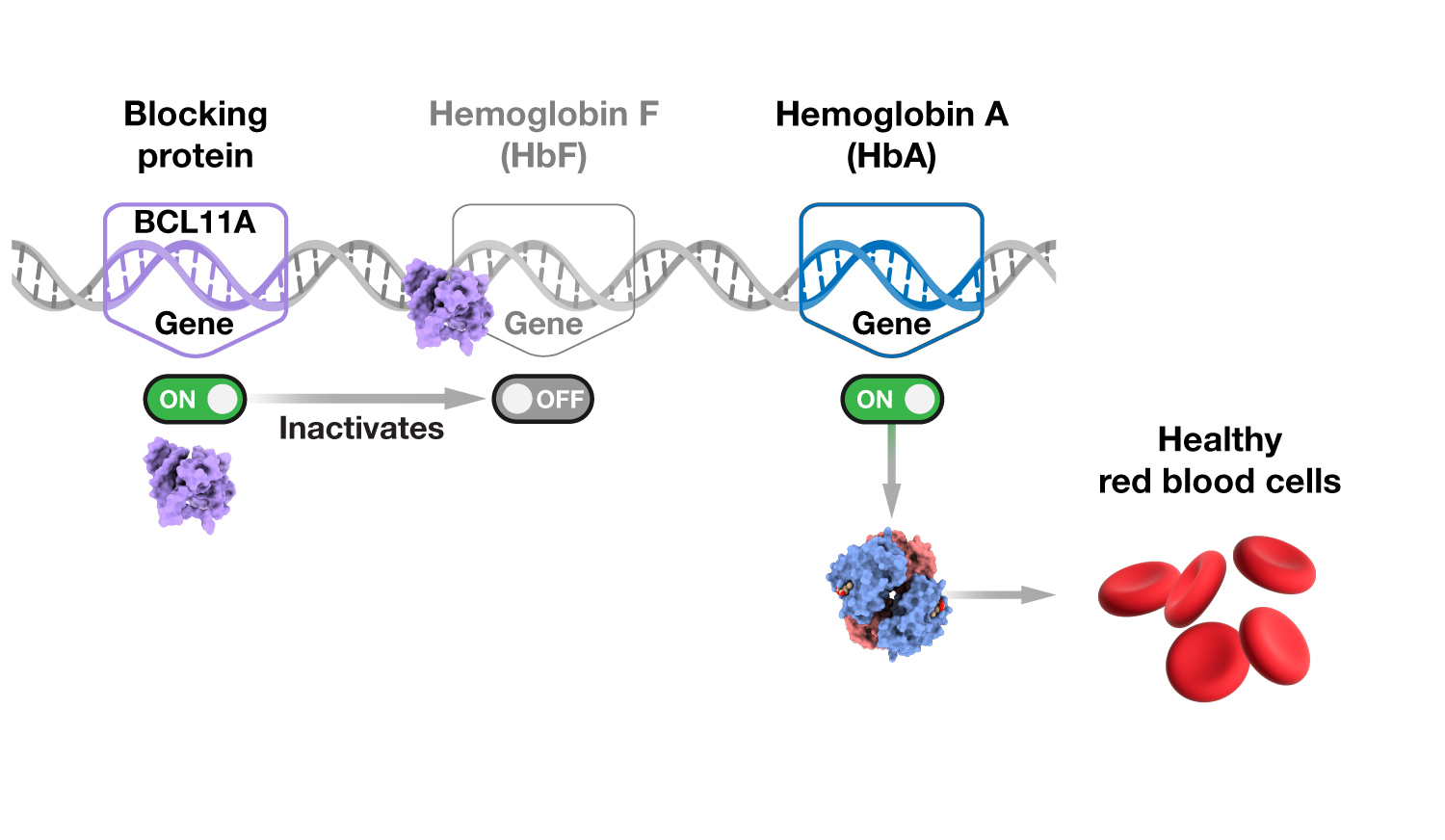
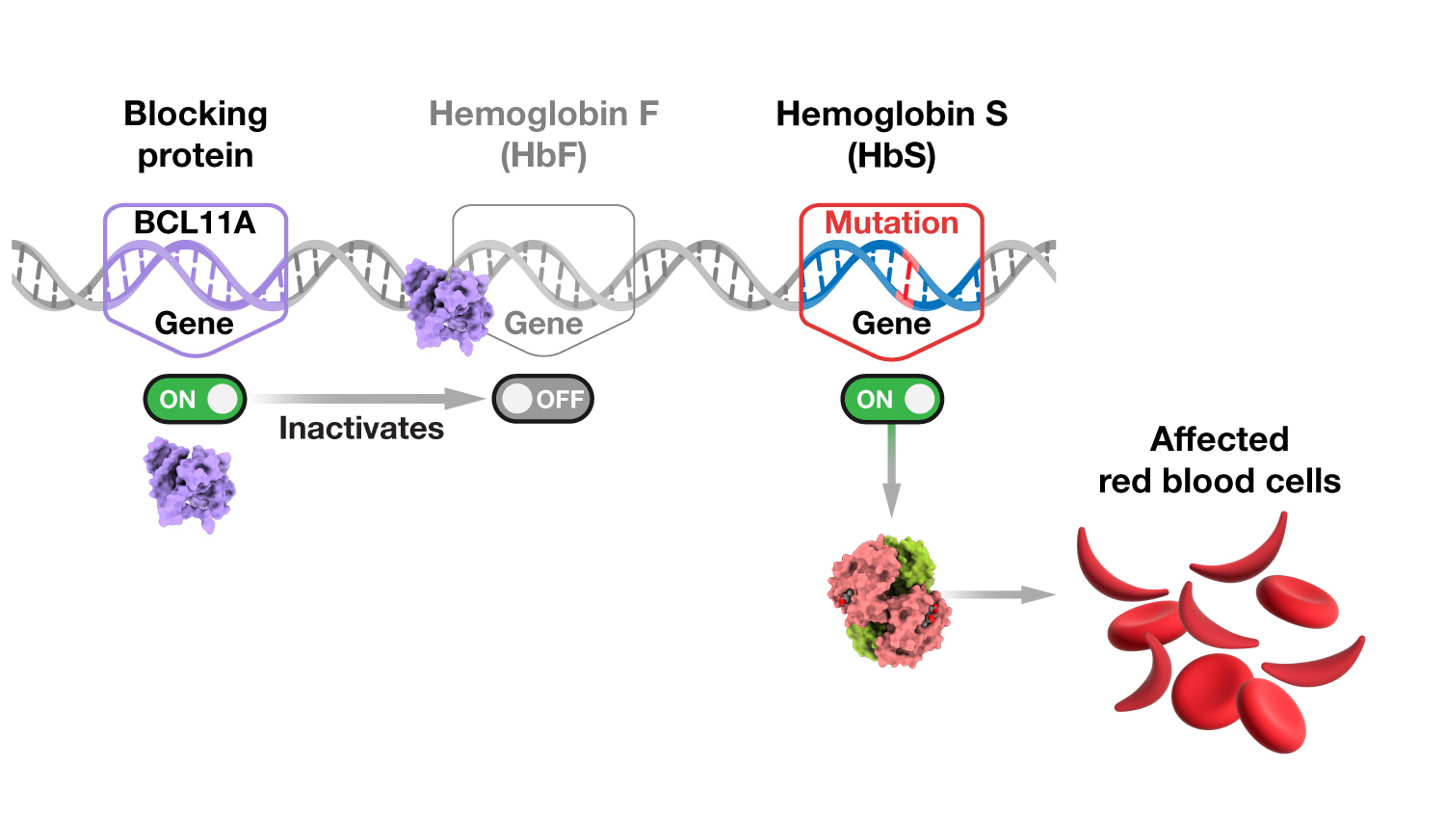
- Hemoglobin F, also known as fetal hemoglobin or HbF, is present in red blood cells before birth (during fetal development). After birth, a gene that codes for a blocking protein (BCL11A) is turned on. BCL11A blocks the production of fetal hemoglobin and tells the body to instead make hemoglobin A. For individuals with sickle cell disease, a small amount of HbF continues to be produced after birth.
- Hemoglobin A, also known as adult hemoglobin or HbA, is typically present in red blood cells after birth.
- Hemoglobin S, also known as sickled hemoglobin or HbS, is an abnormal version of hemoglobin A. Instead of hemoglobin A, the body makes hemoglobin S due to a genetic variant. While hemoglobin S still delivers oxygen, it is not stable and can break apart easily. Hemoglobin S also causes the red blood cells to form a crescent — or sickle — shape.
Sickle cell disease is caused by a genetic variant that makes the body produce hemoglobin S instead of hemoglobin A. You must inherit two variant hemoglobin genes — one for sickle hemoglobin and the other for sickle hemoglobin or another hemoglobin variant (such as hemoglobin C or beta-thalassemia) — to have sickle cell disease. With sickle cell disease, the red blood cells (that are typically round) are sickle-shaped, which causes different health complications.
Comparing hemoglobin types found before and after birth
The Democratizing Education Project welcomes your feedback about the sickle cell disease gene therapy resources. Please email your comments or questions to DemocratizingEd@mail.nih.gov.
These educational materials are for informational purposes only. They are meant to promote your general understanding of gene therapy for sickle cell disease. We encourage you to use these educational materials to talk with your healthcare provider or a clinical trial team.
Last updated: December 12, 2024