NIH researchers develop guidelines for reporting polygenic risk scores
Researchers hope the new approach will be used as a framework for publishing studies on polygenic risk scores.
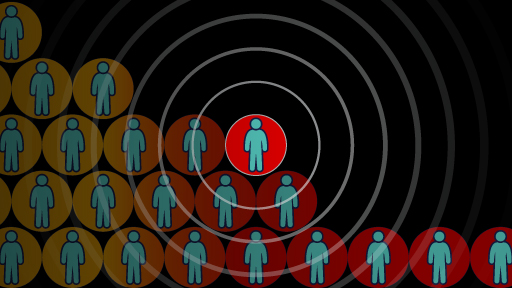
Scientists and healthcare providers are beginning to use a new approach for assessing a person's inherited risk for diseases like Type 2 diabetes, coronary heart disease and breast cancer, which involves calculating a polygenic risk score. The score provides an estimate of an individual’s risk for specific diseases, based on their DNA changes related to those diseases.
Credit: Harry Wedel, NHGRI.
Despite the rise in studies using polygenic risk scores, researchers have observed inconsistencies in how such scores are calculated and reported. These differences threaten to compromise the adoption of polygenic risk scores in clinical care.
To address this concern, the research teams, funded primarily by the National Human Genome Research Institute (NHGRI), have published a 22-item framework in the journal Nature that identifies the minimal polygenic risk score-related information that scientists should include in their studies. This framework — created by NHGRI’s Clinical Genome Resource's (ClinGen) Complex Disease Working Group and the Polygenic Score Catalog (PGS), an open database of polygenic risk scores — will help promote the validity, transparency and reproducibility of polygenic risk scores. NHGRI is part of the National Institutes of Health.
To calculate a person’s polygenic risk score, researchers survey DNA variants in over 6 billion locations in the human genome.
"A real challenge is that the research community has not adopted any universal best practices for reporting polygenic risk scores," said Erin Ramos, Ph.D., a program director for ClinGen, deputy director of the NHGRI Division of Genomic Medicine and co-author of the paper. "With the field growing as fast as it is, we need standards in place so we can meaningfully evaluate these scores and determine which ones are ready to be used in clinical care."
A real challenge is that the research community has not adopted any universal best practices for reporting polygenic risk scores. With the field growing as fast as it is, we need standards in place so we can meaningfully evaluate these scores and determine which ones are ready to be used in clinical care.
This framework builds off another best practice model called the Genetic Risk Prediction Studies (GRIPS) statement, published by an international working group in 2011. GRIPS placed an emphasis on models that included a smaller set of genomic variants and gene scores. However, genetic risk prediction models have evolved rapidly since then, and are based on a much larger set of genomic variants and more complex methodologies. Also, researchers have not fully adopted the GRIPS framework.
"A renewed emphasis on reporting standards by ClinGen and the Polygenic Score Catalog comes at a crucial time for polygenic risk scores," said Genevieve Wojcik, Ph.D., M.H.S., an assistant professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and corresponding author of the paper. "It specifies the minimum information that should be described in a research paper for interpreting a polygenic risk score, reproducing results and eventually translating the information into clinical care."
Some of the new reporting framework items include detailing the study population and the basis for choosing that population.
"If we are to make these scores available to people around the world, the studies need to define who they are studying and why, in the clearest way possible,” said Katrina Goddard, Ph.D., director of Translational and Applied Genomics at the Kaiser Permanente Center for Health Research, Portland, Oregon, who also co-authored the paper. “Without that transparency and reproducibility, efforts to use polygenic risk scores may be undermined."
The new framework suggests that scientists should explain the statistical methods they used to develop and validate the polygenic risk scores. Without a consistent way of reporting polygenic risk scores, it is nearly impossible to compare the utility of the scores for assessing disease risk in people. According to the new guidelines, researchers should also consider potential limitations of these scores and how clinicians should use the scores in patient care.
"If researchers can follow these guidelines, it will be more straightforward to evaluate published polygenic risk scores and decide which ones are a good fit for the clinical setting," said Michael Inouye, Ph.D., director of the Cambridge Baker Systems Genomics Initiative, U.K., and co-senior author of the paper. "For diseases such as breast cancer and many others, we will be able to responsibly place patients in different risk categories and provide beneficial screening strategies and treatments. Ideally, in the future we will detect risk early enough to combat the disease effectively."
ClinGen is funded by NHGRI. Stanford University, an awardee site of the ClinGen consortium, led this effort. The PGS Catalog is funded by the EMBL European Bioinformatics Institute, University of Cambridge, Baker Heart and Diabetes Institute and Health Data Research, U.K.
-
Scientists and healthcare prov...
Scientists and healthcare providers are beginning to use a new approach for assessing a person's inherited risk for diseases like Type 2 diabetes, coronary heart disease and breast cancer, which involves calculating a polygenic risk score. The score provides an estimate of an individual’s risk for specific diseases, based on their DNA changes related to those diseases.
Credit: Harry Wedel, NHGRI.
Despite the rise in studies using polygenic risk scores, researchers have observed inconsistencies in how such scores are calculated and reported. These differences threaten to compromise the adoption of polygenic risk scores in clinical care.
To address this concern, the research teams, funded primarily by the National Human Genome Research Institute (NHGRI), have published a 22-item framework in the journal Nature that identifies the minimal polygenic risk score-related information that scientists should include in their studies. This framework — created by NHGRI’s Clinical Genome Resource's (ClinGen) Complex Disease Working Group and the Polygenic Score Catalog (PGS), an open database of polygenic risk scores — will help promote the validity, transparency and reproducibility of polygenic risk scores. NHGRI is part of the National Institutes of Health.
To calculate a person’s polygenic risk score, researchers survey DNA variants in over 6 billion locations in the human genome.
"A real challenge is that the research community has not adopted any universal best practices for reporting polygenic risk scores," said Erin Ramos, Ph.D., a program director for ClinGen, deputy director of the NHGRI Division of Genomic Medicine and co-author of the paper. "With the field growing as fast as it is, we need standards in place so we can meaningfully evaluate these scores and determine which ones are ready to be used in clinical care."
A real challenge is that the research community has not adopted any universal best practices for reporting polygenic risk scores. With the field growing as fast as it is, we need standards in place so we can meaningfully evaluate these scores and determine which ones are ready to be used in clinical care.
This framework builds off another best practice model called the Genetic Risk Prediction Studies (GRIPS) statement, published by an international working group in 2011. GRIPS placed an emphasis on models that included a smaller set of genomic variants and gene scores. However, genetic risk prediction models have evolved rapidly since then, and are based on a much larger set of genomic variants and more complex methodologies. Also, researchers have not fully adopted the GRIPS framework.
"A renewed emphasis on reporting standards by ClinGen and the Polygenic Score Catalog comes at a crucial time for polygenic risk scores," said Genevieve Wojcik, Ph.D., M.H.S., an assistant professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and corresponding author of the paper. "It specifies the minimum information that should be described in a research paper for interpreting a polygenic risk score, reproducing results and eventually translating the information into clinical care."
Some of the new reporting framework items include detailing the study population and the basis for choosing that population.
"If we are to make these scores available to people around the world, the studies need to define who they are studying and why, in the clearest way possible,” said Katrina Goddard, Ph.D., director of Translational and Applied Genomics at the Kaiser Permanente Center for Health Research, Portland, Oregon, who also co-authored the paper. “Without that transparency and reproducibility, efforts to use polygenic risk scores may be undermined."
The new framework suggests that scientists should explain the statistical methods they used to develop and validate the polygenic risk scores. Without a consistent way of reporting polygenic risk scores, it is nearly impossible to compare the utility of the scores for assessing disease risk in people. According to the new guidelines, researchers should also consider potential limitations of these scores and how clinicians should use the scores in patient care.
"If researchers can follow these guidelines, it will be more straightforward to evaluate published polygenic risk scores and decide which ones are a good fit for the clinical setting," said Michael Inouye, Ph.D., director of the Cambridge Baker Systems Genomics Initiative, U.K., and co-senior author of the paper. "For diseases such as breast cancer and many others, we will be able to responsibly place patients in different risk categories and provide beneficial screening strategies and treatments. Ideally, in the future we will detect risk early enough to combat the disease effectively."
ClinGen is funded by NHGRI. Stanford University, an awardee site of the ClinGen consortium, led this effort. The PGS Catalog is funded by the EMBL European Bioinformatics Institute, University of Cambridge, Baker Heart and Diabetes Institute and Health Data Research, U.K.
About NHGRI and NIH
The National Human Genome Research Institute (NHGRI) is one of the 27 institutes and centers at the NIH, an agency of the Department of Health and Human Services. The NHGRI Division of Intramural Research develops and implements technology to understand, diagnose and treat genomic and genetic diseases. Additional information about NHGRI can be found at: www.genome.gov.
The National Institutes of Health (NIH) is the nation's medical research agency, includes 27 institutes and centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical and translational medical research, and is investigating the causes, treatments and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
Press Contact
Last updated: March 10, 2021