Pras E, Aksentijevich I, Gruberg L, Balow JE Jr, Prosen L, Dean M, Steinberg AD, Pras M, Kastner DL. Mapping of a gene causing familial Mediterranean fever to the short arm of chromosome 16. N Engl J Med, 326:1509-1513. 1992. [PubMed]
International FMF Consortium (Kastner DL, corresponding author). Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. Cell, 90:797-807. 1997. [PubMed]
McDermott MF, Aksentijevich I, Galon J, McDermott EM, Ogunkolade BW, Centola M, Mansfield E, Gadina M, Karenko L, Pettersson T, McCarthy J, Frucht DM, Aringer M, Torosyan Y, Teppo A-M, Wilson M, Karaarslan HM, Wan Y, Todd I, Wood G, Schlimgen R, Kumarajeewa TR, Cooper SM, Vella JP, Amos CI, Mulley J, Quane KA, Molloy MG, Ranki A, Powell RJ, Hitman GA, O'Shea JJ, Kastner DL. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell, 97:133-144. 1999. [PubMed]
Aksentijevich I, Nowak M, Mallah M, Chae JJ, Watford WT, Hoffman SR, Stein L, Russo R, Goldsmith D, Dent P, Rosenberg HF, Austin F, Remmers EF, Balow JE Jr, Rosenzweig S, Komarow H, Shoham NG, Wood G, Jones J, Mangra N, Carrero H, Adams BS, Moore TL, Schikler K, Hoffman H, Lovell DJ, Lipnick R, Barron K, O'Shea JJ, Kastner DL, Goldbach-Mansky R. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrin-associated autoinflammatory diseases. Arthritis Rheum, 46:3340-3348. 2002. [PubMed]
Shoham NG, Centola M, Mansfield E, Hull KM, Wood G, Wise CA, Kastner DL. Pyrin binds the PSTPIP1/CD2BP1 protein, defining PAPA syndrome and familial Mediterranean fever as disorders in the same pathway. Proc Natl Acad Sci USA, 100:13501-13506. 2003. [PubMed]
Goldbach-Mansky R, Dailey NJ, Canna SW, Gelabert A, Jones J, Rubin BI, Kim HJ, Brewer C, Zelewski C, Wiggs E, Hill S, Turner ML, Karp BI, Aksentijevich I, Pucino F, Penzak S, Haverkamp MH, Stein L, Adams BS, Moore TL, Fuhlbrigge RC, Shaham B, Jarvis JN, O'Neill K, Vehe RK, Beitz LO, Gardner G, Hannan WP, Warren RW, Horn W, Cole JL, Paul SM, Hawkins PN, Pham TH, Snyder C, Wesley RA, Hoffman SC, Holland SM, Butman JA, Kastner DL. Neonatal onset multisystem inflammatory disease responsive to IL-1b inhibition. N Engl J Med, 355:581-592. 2006. [PubMed]
Remmers EF, Plenge RM, Lee AT, Graham RR, Hom G, Behrens TW, deBakker PIW, Le JM, Lee H-Y, Batliwalla F, Li W, Masters SL, Booty MG, Carulli JP, Padyukov L, Alfredsson L, Klareskog L, Chen WV, Amos CI, Criswell LA, Seldin MF, Kastner DL, Gregersen PK. A variant form of STAT4 increases genetic susceptibility to rheumatoid arthritis and systemic lupus erythematosus. N Engl J Med, 357:997-986. 2007. [PubMed]
Remmers EF, Plenge RM, Lee AT, Graham RR, Hom G, Behrens TW, de Bakker PIW, Le JM, Lee H-S, Batliwalla F, Li W, Masters SL, Booty MG, Carulli JP, Padyukov L, Alfredsson L, Klareskog L, Chen WV, Amos CI, Criswell LA, Seldin MF, Kastner DL, Gregersen PK. STAT4 and the risk of rheumatoid arthritis and systemic lupus erythematosus. N Engl J Med, 357:977-986. 2007. [PubMed]
Aksentijevich I, Masters SL, Ferguson PJ, Dancey P, Frenkel J, van Royen-Kerkhoff A, Laxer R, Tedgård U, Cowen EW, Pham T-H, Booty M, Estes JD, Sandler NG, Plass N, Stone D, Turner ML, Hill S, Butman JA, Schneider R, Babyn P, El-Shanti HI, Pope E, Barron K, Bing X, Laurence A, Lee C-CR, Chapelle D, Clarke GI, Ohson K, Nicholson M, Gadina M, Yang B, Korman BD, Gregersen PK, van Hagen M, Hak AE, Huizing M, Rahman P, Douek DC, Remmers EF, Kastner DL, Goldbach-Mansky R. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med, 360:2426-2437. 2009. [PubMed]
Remmers EF, Cosan F, Kirino Y, Ombrello MJ, Abaci N, Satorius C, Le JM, Yang B, Korman BD, Cakris A, Aglar O, Emrence Z, Azakli H, Ustek D, Tugal-Tutkun I, Akman-Demir G, Chen W, Amos CI, Dizon MB, Kose AA, Azizlerli G, Erer B, Brand OJ, Kaklamani VG, Kaklamanis P, Ben-Chetrit E, Stanford M, Fortune F, Ghabra M, Ollier WER, Cho Y-H, Bang D, O'Shea J, Wallace GR, Gadina M, Kastner DL, Gül A. Genome-wide association study identifies variants in the MHC class I, IL10, and IL23R-IL12RB2 regions associated with Behçet's disease. Nature Genet, 42:698-702. 2010. [PubMed]
Bulua AC, Simon A, Maddipati R, Pelletier M, Park H. Kim K-Y, Sack MN, Kastner DL, Siegel RM. Mitochondrial reactive oxygen species promote production of pro-inflammatory cytokines and are elevated in a TNFR1-associated periodic syndrome (TRAPS). J Exp Med, 208:519-533. 2011. [PubMed]
Stojanov S, Lapidus S, Chitkara P, Feder H, Salazar JC, Fleisher TA, Brown MR, Edwards KM, Ward MM, Colbert RA, Sun H-W, Wood GM, Barham BK, Jones A, Aksentijevich I, Goldbach-Mansky R, Athreya B, Barron KS, Kastner DL. Periodic fever, aphthous stomatitis, pharyngitis, and adenitis (PFAPA) is a disorder of innate immunity and Th1 activation responsive to IL-1 blockade. Proc Natl Acad Sci USA, 108:7148-7153. 2011. [PubMed]
Chae JJ, Cho Y-H, Lee G-S, Cheng J, Liu PP, Feigenbaum L, Katz SI, Kastner DL. Gain-of-function pyrin mutations induce NLRP3 protein-independent interleukin-1b activation and severe autoinflammation in mice. Immunity, 34;755-768. 2011. [PubMed]
Ombrello MJ, Remmers EF, Sun G, Freeman AF, Datta S, Torabi-Parizi P, Subramanian N, Bunney TD, Baxendale RW, Romberg N, Komarow H, Aksentijevich I, Kim HS, Ho J, Cruse G, Jung MY, Gilfillian A, Metcalfe DD, Nelson C, O'Brien M, Wisch L, Stone K, Douek DC, Gandhi C, Wanderer AA, Lee H, Nelson S, Shianna KV, Cirulli ET, Goldstein DB, Long EO, Moir S, Meffre E, Holland S, Kastner DL, Katan M, Hoffman HM, Milner JD. Cold urticaria, immunodeficiency, and autoimmunity related to PLCG2 deletions. N Engl J Med, 366:330-338. 2012. [PubMed]
Zhou Q, Lee G-S, Brady J, Sheikh A, Katan M, Martins MS, Bunney TD, Datta S, Milner J, Ombrello A, Stone D, Ombrello MJ, Khan J, Kastner DL, Aksentijevich I. Exome sequencing identifies a hypermorphic missense mutation in the PLCG2 gene as the cause of a dominantly inherited autoinflammatory disease with immunodeficiency. Am J Hum Genet, 91:713-720. 2012. [PubMed]
Lee G-S, Subramanian N, Kim A, Aksentijevich I, Goldbach-Mansky R, Sacks DB, Germain RN, Kastner DL, Chae JJ. The calcium-sensing receptor regulates the NLRP3 inflammasome through intracellular Ca2+ and cAMP. Nature 492:123-127, 2012. [PubMed]
Kirino Y, Bertsias G, Ishigatsubo Y, Mizuki N, Tugal-Tutkun I, Seyahi E, Ozyazgan Y, Sacli FS, Erer B, Inoko H, Emrence Z, Cakar A, Abaci N, Ustek D, Satorius C, Ueda A, Takeno M, Kim Y, Wood GM, Ombrello MJ, Meguro A, Gül A, Remmers EF, Kastner DL. Genome-wide association analysis identifies new susceptibility loci for Behçet's disease and epistasis between HLA-B*51 and ERAP1. Nature Genet, 45:202-207. 2013. [PubMed]
Kirino Y, Zhou Q, Ishigatsubo Y, Mizuki N, Tugal-Tutkun I, Seyahi E, Ozyazgan Y, Ugurlu S, Erer B, Abaci N, Ustek D, Meguro A, Ueda A, Takeno M, Inoko H, Ombrello MJ, Satorius C, Maskeri B, Mullikin JC, Sun H-W, Gutierrez-Cruz G, Kim Y, Wilson AF, Kastner DL, Gül A, Remmers EF. Targeted resequencing implicates the familial Mediterranean fever gene MEFV and the toll-like receptor 4 gene TLR4 in Behçet's disease. Proc Natl Acad Sci USA, 110:8134-8139. 2013. [PubMed]
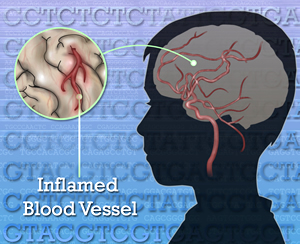
Zhou Q, Yang D, Ombrello AK, Zavialov AV, Toro C, Zavialov AV, Stone DL, Chae JJ, Rosenzweig SD, Bishop K, Barron K, Kuehn HS, Hoffmann P, Negro A, Tsai WL, Cowen EW, Pei W, Milner JD, Silvin C, Heller T, Chin DT, Patronas NJ, Barber JS, Lee C-CR, Wood GM, Ling A, Kelly SJ, Kleiner DE, Mullikin J, Ganson NJ, Kong HH, Hambleton S, Candotti F, Quezado MM, Calvo K, Alao H, Barham BK, Jones A, Meschia JF, Worrall BB, Kasner SE, Rich SS, Goldbach-Mansky R, Abinum M, Chalom E, Gotte AC, Punaro M, Pascual V, Verbsky J, Torgerson TR, Singer NG, Gershon TR, Ozen S, Karadag O, Fleisher TA, Remmers EF, Burgess SM, Moir SL, Gadina M, Sood R, Hershfield M, Boehm M, Kastner DL, Aksentijevich I. Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med, 370:911-920. 2014. [PubMed]
Ombrello MJ, Kirino Y, de Bakker PI, Gül A, Kastner DL, Remmers EF. Behçet disease-associated MHC class I residues implicate antigen binding and regulation of cell-mediated cytotoxicity. Proc Natl Acad Sci USA, 111:8867-8872. 2014. [PubMed]
Zhou Q, Wang H, Schwartz DM, Stoffels M, Park YH, Zhang Y, Yang D, Demirkaya E, Takeuchi M, Tsai WL, Layons JJ, Yu X, Ouyang C, Chen C, Chin DT, Zaal K, Chandrasekharappa SC, Hanson EP, Yu Z, Mullikin JC, Hasni SA, Wertz IE, Ombrello AK, Stone DL, Hoffmann P, Jones A, Barham BK, Leavis HL, van Royen-Kerkof A, Sibley C, Batu ED, Gül A, Siegel RM, Boehm M, Milner JD, Ozen S, Gadina M, Chae J, Laxer RM, Kastner DL, Aksentijevich I. Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nature Genet, 48:67-73. 2016. [PubMed]
Boyden SE, Desai A, Cruse G, Young ML, Bolan HC, Scott LM, Eisch AR, Long RD, Lee C-CR, Satorius CL, Pakstis AJ, Olivera A, Mullikin JC, Chouery E, Mégarbané, Medlej-Hashim M, Kidd KK, Kastner DL, Metcalfe DD, Komarow HD. Vibratory urticaria associated with a missense variant in ADGRE2. N Engl J Med, 375(1):95. 2016. [PubMed]
Chung LK, Park YH, Zheng Y, Brodsky IE, Hearing P, Kastner DL, Chae JJ, Bliska JB. The Yersinia Virulence Factor YopM Hijacks Host Kinases to Inhibit Type III Effector-Triggered Activation of the Pyrin Inflammasome. Cell Host Microbe, 20(3):296-306. 2016. [PubMed]
Stoffels M, Kastner DL Old dogs, new tricks: monogenic autoinflammatory disease unleashed. Annu Rev Genom Hum Genet, 17:18.1-18.28. 2016. [PubMed]
Zhou Q, Yu X, Demirkaya E, Deuitch N, Stone D, Tsai WL, Kuehn HS, Wang H, Yang D, Park YH, Ombrello AK, Blake M, Romeo T, Remmers EF, Chae JJ, Mullikin JC, Güzel F, Milner JD, Boehm M,Rosenzweig SD, Gadina M, Welch SB, Özen S, Topaloglu R, Abinum M, Kastner DL, Aksentijevich I. Biallelic hypomorphic mutations in a linear deubiquitinase define otulipenia, an early-onset autoinflammatory disease. Proc Natl Acad Sci USA, 113:10127-10132. 2016. [PubMed]
Park YH, Wood G, Kastner DL, Chae JJ (2016) Pyrin inflammasome activation and RhoA signaling in the autoinflammatory diseases FMF and HIDS. Nat Immunol, 17:914-921. 2016. [PubMed]
Takeuchi M, Mizuki N, Meguro A, Ombrello MJ, Kirino Y, Satorius C, Le J, Blake M, Erer B, Kawagoe T, Ustek D, Tugal-Tutkun I, Seyahi E, Ozyazgan Y, Sousa I, Davatchi F, Francisco V, Shahram F, Abdollahi BS, Nadji A, Shafiee NM, Ghaderibarmi F, Ohno S, Ueda A, Ishigatsubo Y, Gadina M, Oliveira SA, Gül A, Kastner DL, Remmers EF. Dense genotyping of immune-related loci implicates host responses to microbial exposure in Behçet's disease susceptibility. Nat Genet, 49:438-443. 2017. [PubMed]
Manthiram K, Zhou Q, Aksentijevich I, Kastner DL. The monogenic autoinflammatory diseases define new pathways in human innate immunity and inflammation. Nat Immunol. 18:832-842. 2017. [PubMed]
Ombrello AK, Qin J, Hoffmann P, Kuman P, Stone D, Jones A, Romeo T, Barham B, Pinto-Patarroyo G, Toro C, Soldatos A, Zhou Q, Deuitch N, Aksentijevich I, Sheldon SL, Kelly S, Man A, Barron K, Hershfield M, Flegel WA, Kastner DL. Treatment strategies for the deficiency of adenosine deaminase 2. N Engl J Med 380:1582-1584. 2019. [PubMed]
Lalaoui N, Boyden SE, Oda H, Wood GM, Stone DL, Chau D, Liu L, Stoffels M, Kratina T, Lawlor KE, Zaal KJM, Hoffmann PM, Etemadi N, Shield-Artin K, Biben C, Tsai WL, Blake MD, Kuehn HS, Yang D, Anderton H, Silke N, Wachsmuth L, Zheng L, Sampaio Moura N, Beck DB, Gutierrez-Cruz G, Ombrello AK, Pinto-Patarroyo GP, Kueh AJ, Herold MJ, Hall C, Wang H, Chae JJ, Dmitrieva NI, McKenzie M, Light A, Barham BK, Jones A, Romeo TM, Zhou Q, Aksentijevich I, Mullikin JC, Gross AJ, Shum AK, Hawkins ED, Masters S, Lenardo MJ, Boehm M, Rosenzweig SD, Pasparakis M, Voss AK, Gadina M, Kastner DL, Silke J. Mutations that prevent caspase-8 cleavage of RIPK1 cause inflammation in humans and mouse. Nature 577:103-108. 2020.